ITU's work has covered both telemedicine and e-health, through on-the-ground interventions in developing countries and clinics and hospitals.
Under Resolution ITU-R 67-1 (Geneva 2019)-“Telecommunication/ICT accessibility for persons with disabilities and persons with specific needs", ITU-R conducts studies, research, guidelines and recommendations related to telecommunication/ICT accessibility for persons with disabilities and persons with specific needs, taking into account Resolutions 191 (Rev. Dubai, 2018) and 200 (Rev. Dubai, 2018) of the ITU Plenipotentiary Conference, in close cooperation with ITU-T and ITU-D.
ITU-R promotes wireless and broadcasting technological development though the production of Recommendations, Reports and Questions relating to people with disabilities, and by so doing to improving their accessibility and to reducing the overall Digital Disabilities Divide. So far, a number of deliverables pertinent to accessibility matters were published (see the page of
ITU-R Sector contribution to Bridging the Digital Disabilities Divide).
ITU-T has published
ICT standards related to e-health for developing countries and the use of ICTs, health information issued by WHO or other UN agencies relating to e-health, its opportunities and potential risks. ITU-T Study Group 16's work evolves in line with industry needs and the group is accelerating its development of standards for e-health, accessibility and Intelligent Transport Systems (ITS). In collaboration with WHO and with other Standards Development Organizations (SDOs), e-health standardization work is active in areas such as safe listening; brain informatics; UHD medical imaging; and personal connected health.
ITU-T Study Group 16 also hosts the ITU/WHO
Focus Group on Artificial Intelligence for Health (FG-AI4H), established in mid-2018. This Focus Group works in partnership with the WHO to establish a standardized assessment framework for the evaluation of AI-based methods for health, diagnosis, triage or treatment decisions. FG-AI4H recently established a new ad hoc Group on “Digital Technologies for COVID Health Emergencies" (AHG-DT4HE), which reviews the role of AI and other digital technologies in combatting COVID-19 throughout an epidemic's life cycle to learn how to best leverage digital technologies to successfully manage future health emergencies.
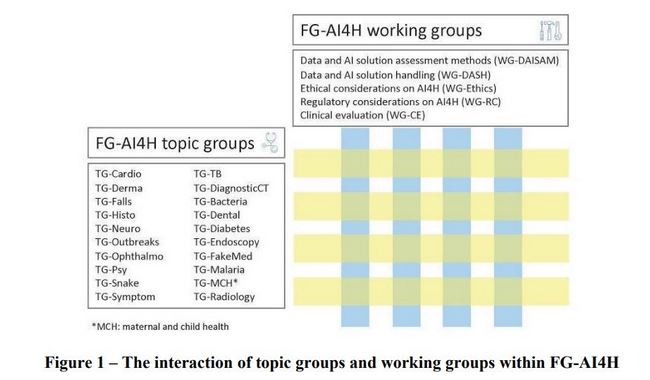
Source: Whitepaper
for the ITU/WHO Focus Group on Artificial Intelligence for Health.
ITU has also partnered with the WHO to bring together governments, health professionals, academia and the industry to discuss how ICTs can help make listening safe. Expected outcomes include policy briefs, international standards, and awareness campaigns to ensure that people of all ages can enjoy music, games, movies and live events without jeopardizing their hearing. ITU-T leads the development of technical standards for devices (such as mobile phones) as ITU-T H. 870 series that would allow for safe listening. When implemented, these standards will allow controlling exposure to loud sounds through personal audio systems and will provide information that enable users to make safe listening choices.
The Continua Design Guidelines are approved as ITU-T H.810 series on personal health systems which define a framework of underlying standards and criteria that are required to ensure the interoperability of components used for applications monitoring personal health and wellness. They also contain design guidelines (DGs) that further clarify the underlying standards or specifications by reducing options or by adding missing features to improve interoperability.
In 1990, ITU-T also pioneered various accessibility standardization work with Recommendation V.18 on a multi-function text telephone for deaf communication. Since then, ITU-T continues to engage through its standardization work to ensure equitable access to telecommunication through new and old technologies – see the
backgrounder on accessibility.
In 2012, in conjunction with WHO, ITU-D launched the 'Be he@lthy, be mobile programme', which works with governments to introduce evidence-based mHealth services into national health systems, institutionalize them nationally on a large-scale, evaluate their impact, and share best practices. This initiative continues to support programmes in a combination of low-, middle- and high-income countries, sharing content and experiences between them to accelerate the adoption of best practices. It aims to: help countries implement and sustainably scale mHealth programmes; develop validated content that works; enter into meaningful partnerships globally and in country for multisectoral and ecosystem approaches; explore and expand innovations; share knowledge; and build country capacity for innovation management and institutionalize digital health .
In collaboration with the WHO, ITU-D has worked on
National eHealth Strategy Toolkit in 2012. The National eHealth Strategy Toolkit is an expert, practical guide that provides governments, their ministries and stakeholders with a solid foundation and method for the development and implementation of a national eHealth vision, action plan and monitoring framework. ITU has also published the
Digital Health Platform handbook about architectures for digital health systems. ITU has also partnered with the WHO and Andalusian Ministry on the
mhealth hub, which aims to: collect expertise on mHealth in Europe; assist countries in implementing mHealth strategies; facilitate innovation in mHealth; help accelerate the EU Digital Single Market; to produce knowledge tools for health systems and services on NCDs; and to provide a code of ethics for mHealth data.
In 2018, ITU-D Study Group 2 examined
Question 2/2 on Telecommunications/ICTs for eHealth, and covered issues such as e-health activities carried out by the BDT in cooperation with other UN agencies, such as WHO, in the field of non-infectious disease, infectious disease, including pandemics, and mother and child in particular. In conjunction with ITU-T, ITU-D has explored guidelines on collecting and managing big data for public health crises, as well as new technologies.
Last update: January 2021